Pediatric Glasgow Coma Scale Pdf For Printing
Extraordinary efforts have been made by the authors, the editor and the publisher of the National Center of Continuing Education, Inc. Courses to ensure dosage recommendations and treatments are precise and agree with the highest standards of practice. However, as a result of accumulating clinical experience and continuing laboratory studies, dosage schedules and/or treatment recommendations are often altered or discontinued.
RSI RAPID SEQUENCE INTUBATION. Trauma patients with Glasgow Coma Scale of nine or less with gag reflex. Current Printing: September 8.
In all cases the advice of a physician should be sought and followed concerning initiating or discontinuing all medications or treatments. The planner(s), author(s) and/or editor(s) of each course have attested to no conflict of interest nor bias on the subject. The National Center of Continuing Education, Inc. Does not accept commercial support on any course nor do they endorse any products that may be mentioned in the course. Any off-label use for medications mentioned in a course is identified as such. No part of this publication may be reproduced stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise without the prior written permission of the publisher.
This course expired Oct 31, 2015 and is no longer available for purchase. Tragedy of Shaken Baby Syndrome: Preventing Abusive Head Trauma Authors: Cheryl Duksta, RN, ADN, M.Ed Shelda L. Hudson, RN, BSN, PHN The purpose of this course is to educate healthcare professionals in prevention of and intervention of pediatric abusive head trauma (PAHT), particularly shaken baby syndrome (SBS). Child abuse and trauma affect the entire family unit, the healthcare system, and the community as a whole. The goal of this course is to prepare nurses to care for patients who have suffered from SBS and educate their families about prevention of this type of trauma. Course objectives include:. Summarize the mechanism of injury of pediatric abusive head trauma.
Discriminate the signs and symptoms of SBS. Describe the diagnosis of and treatment for SBS Exceeds Mandatory Kentucky requirement. To be completed before December 2013 About the Authors Cheryl Duksta, RN, ADN, MEd, is currently a critical care nurse in an intermediate care unit in Austin, Texas. She is an active member of the American Association of Critical-Care Nurses (AACN) Greater Austin chapter. A master's prepared teacher and former public school teacher, Ms. Duksta frequently serves as a continuing education facilitator.
She has 15 years of experience in education and medical publishing, including writer and editor at the National Center of Continuing Education, Inc. Hudson, RN, BSN, PHN, completed her bachelor's degree in nursing and obtained a public health certificate at Azusa Pacific University and is a past member of the International Association of Forensic Nurses (IAFN). She is the Nurse Supervisor of the Instructional Systems Development department of the National Center of Continuing Education, Inc. In this capacity, she is responsible for directing the activities of this department; selecting qualified, credentialed authors for the courses offered by the National Center; and advising staff of required course design and criteria. Hudson has more than 20 years of experience in publishing courses in continuing education for healthcare professionals with the National Center. Purpose and Goals. The purpose of this course is to educate healthcare professionals in prevention of and intervention of pediatric abusive head trauma (PAHT), particularly shaken baby syndrome (SBS).
Child abuse and trauma affect the entire family unit, the healthcare system, and the community as a whole. The goal of this course is to prepare nurses to care for patients who have suffered from SBS and educate their families about prevention of this type of trauma. Instructional Objectives Upon completion of this course, the learner will be able to:. Define shaken baby syndrome (SBS).
Summarize the mechanism of injury of pediatric abusive head trauma. Discriminate the signs and symptoms of SBS. Outline the causes of and risk factors for SBS.
Describe the diagnosis of and treatment for SBS. Explain pertinent parent education as related to SBS. Evaluate resources for healthcare personnel and parents regarding SBS. Introduction Connie, a nurse at a pediatrics office, called back her first patient of the morning, a 4-month-old boy named Joshua whose parents brought him in for lethargy and poor feeding.
During the medical history, Joshua's parents explained that Joshua had been unusually 'groggy' for the past 2 days and had not been waking to eat in his typical feeding pattern. When they managed to rouse him enough to take a bottle, he couldn't obtain good suction, so his intake was poor. Joshua's mother stated, 'I think he may have caught a virus from his uncle, who babysat Joshua the other night.
Joshua's been like this ever since we went out to dinner and left him with my brother. But I've taken his temperature routinely, and he hasn't been running a fever.'
Connie scanned the baby's body when his parents undressed him and while she took his vital signs. Joshua had faint bruises bilaterally on his arms.
When asked, Joshua's parents said that his uncle made the bruises while bouncing Joshua on his knee. These subtle signs alerted Connie to the possibility of a traumatic brain injury caused by shaking a baby.
Connie documented her assessment and quickly informed the doctor of a possible case of SBS. The doctor immediately assessed Joshua, explained to the parents that further diagnostics needed to be conducted, and called an ambulance to transport Joshua to the local hospital.
Although they didn't know for sure if Joshua had suffered abuse, Connie and the doctor felt confident that they had taken steps necessary to assist Joshua in the event that he did suffer from SBS. Child abuse and SBS did not originate in modern times. Pediatric abusive head trauma can be found in records from biblical times.
In 1971, pediatric neurosurgeon Dr. Norman Guthkelch described the brain damage related to shaken baby syndrome, and in 1972, Dr. John Caffey coined the term whiplash shaken baby syndrome.
In the 1980s, the term shaken baby syndrome was first used and has since been widely adopted by the public to describe this distinctive form of abuse. SBS, also known as shaken-impact syndrome and inflicted head injury, is a form of abusive head trauma that includes a constellation of signs and symptoms that result from violently shaking an infant by the shoulders, arms, or legs.
Infant Glasgow Coma Scale
Injury may result from shaking alone or from shaking combined with impact, such as when an infant is thrown against a wall. Although SBS can occur in children up to 5 years old, it is most common in infants younger than 12 months, especially those between 2 and 4 months of age. The actual number of SBS cases is not known; however, experts estimate 1,200–1,400 cases of severe or fatal head trauma occur each year in the United States. SBS is the most common cause of death and long-term disability in physically abused infants and young children.
Of infants who are shaken, 25% will die, and almost all victims will suffer serious health consequences, including closed head injuries, spinal cord injuries, partial or total blindness, developmental delays or learning deficits, cerebral palsy, seizure disorders, hearing loss, and mental retardation. Mechanism of Injury Infants and toddlers are prone to head injuries because of the relatively large size of their head. In particular, babies have large, heavy heads and weak neck muscles. Their undeveloped brains have a higher water content compared with adult brains. When an infant is shaken, the infant's head whips forward and backward, causing the fragile brain to slosh back and forth, compressing and contorting within the infant's skull.
This acceleration/deceleration movement can cause bruising, swelling, and bleeding. During the abuse, the infant's head may strike an object, or the infant may be thrown down to the floor or against a wall, resulting in blunt trauma.
Studies have shown that the force of deceleration is greater with impact, compared to simply shaking. Because this type of injury is unique to shaking abuse, some experts suggest that the term shaken-impact syndrome is more accurate for this type of trauma. Subdural and subarachnoid hemorrhage (bleeding in the brain), retinal hemorrhage (bleeding in the retina), diffuse axonal injury (nerve damage), damage to the spinal cord and neck, and fractures of the ribs and bones are characteristic injuries of SBS. Although all of these injuries may be present in cases of SBS, the triad of injuries that points to SBS is subdural hemorrhage, retinal hemorrhage, and cerebral edema.
Subdural hemorrhage that occurs with SBS occurs between the dura and the surface of the brain. The bridging vessels that transport blood from the surface of the brain to the dura are delicate in infants and susceptible to tearing when sudden head motions extend the vessels. Subdural hemorrhage can be either unilateral or bilateral, although it is more commonly a bilateral injury. Autopsies of infants who are shaken reveal cerebral edema and bleeds ranging from 2–15 ml in volume, compared with more than 100 ml in cases of accidental head injury.
The same vessels that tear to produce a subdural hemorrhage can also produce a subarachnoid bleed because they pass through the arachnoid space, which is greater in infants than in adults. Subarachnoid hemorrhage is commonly sparse and often difficult to detect. If the infant suffers a head impact along with shaking, the force from the blow often results in diffuse brain swelling and increased intracranial pressure because the compliant skull provides less protection for a child than the developed skull does for an adult. A cardinal sign of SBS is retinal hemorrhage, which is noted in 70–85% of the cases of abusive head injury due to acceleration/deceleration forces. The forceful shaking associated with SBS causes the retina to split, allowing blood to fill the empty cavity, which may result in blindness.
Diffuse axonal injury causes the potentially profound disability associated with SBS. Because the axons of infants have not developed myelin, they are more susceptible to tearing. The acceleration/deceleration movements of the head related to shaking tear the axons, resulting in cell death and brain swelling. Because infants have such small axonal processes, these types of injuries can be difficult to detect. Abusive head injuries may be accompanied by outward signs of abuse, such as bruising, or fractures that can be seen on x-ray. Too often, however, injuries due to SBS are insidious and not easily noticed by caregivers or healthcare professionals. Symptoms of SBS range from vague, such as lethargy, vomiting, and crying, to severe and frightening, such as convulsions and coma.
(See Figure 1 for a detailed list of signs and symptoms of SBS.). Signs and Symptoms of SBS Not all injuries from SBS are visible; however, babies may display these outward signs:. Vomiting. Increased irritability or uncontrollable crying. Poor sucking resulting in an inability to nurse or eat. Significant changes in sleeping patterns.
Bulging fontanelles, separated skull sutures, or increased head circumference. Convulsions or seizures. Respiratory distress. Unresponsiveness or inability to be awakened. Coma or death The injuries associated with SBS result from extreme force.
Subdural and retinal hemorrhages are not injuries related to short falls in the home, motions associated with an infant swing, bouncing of infants on a knee, or playful tossing of infants. These injuries are associated with rotational forces from violent shaking. Causes and Risk Factors Prolonged or inconsolable crying is the most common trigger for SBS. Episodes of crying that can trigger shaking behavior among parents and caregivers are known to increase in the first month after birth, peak in the second month, and decrease thereafter. Because young infants cry more frequently than older infants and toddlers, they are more at risk for being shaken. Many caregivers deal with crying with patience and compassion; however, at times caregivers may be under stress from work, family, or financial issues; in addition, they may be suffering from the exhaustion related to parenting.
Add the frustration of an inconsolable baby, and caregivers can 'snap.' In addition to crying, other situations can trigger SBS, including feeding difficulties, such as when infants refuse to take a bottle, and toilet training in older infants. These situations can increase caregiver frustration and anger and make them susceptible to shaking their infant. Certain risk factors put an infant at risk for SBS. Children are more at risk for SBS if their parent or caregiver:. is younger. abuses drugs or alcohol.
has an unstable support system. has unrealistic expectations about childrearing and child development. was abused or neglected as a child. was the victim of or witnessed domestic violence. is a single parent.
Parents of premature infants, infants with disabilities, and infants who are younger than 6 months of age are more likely to respond to their infant with shaking. Parents of multiple infants, such as twins, are also at higher risk for this behavior. Gender plays a role in risk. Boys are more likely to be shaken than girls. One study showed that almost two thirds of shaken infants were boys. Biological parents are the most common perpetrators, with boyfriends of mothers the next most likely abusers.
In the past, men were thought to be the main perpetrators of shaking abuse, but recent research suggests that women are just as likely to shake their infants. Because society views mothers as nurturing caregivers, they are suspected of abuse less frequently, even though they are just as likely to inflict trauma as their male counterparts. When comparing the extent of injuries, however, men cause more traumatic injury when they shake an infant because they are physically stronger than women. Diagnosis and Treatment Diagnosing shaken baby syndrome can be difficult due to the unique nature of the trauma and the age of the victim.
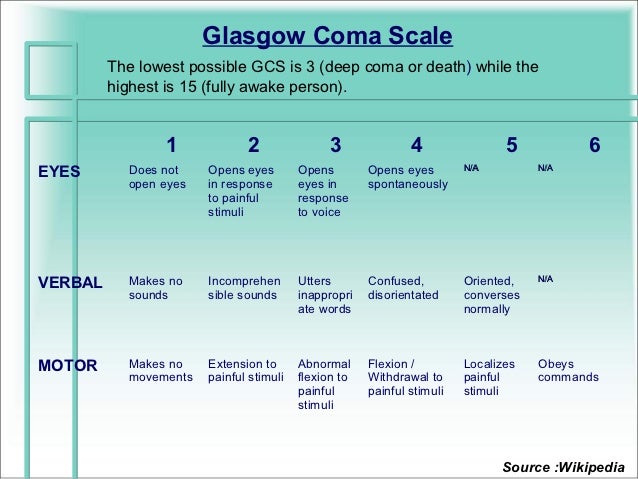
Because infants are more tolerant of increased intracranial pressure, related signs and symptoms are sometimes delayed, postponing diagnosis. Also, it is difficult to assess signs of head injury in children because of their developmental level, with the Glasgow Coma Scale being an unreliable measurement of their level of impairment. A modified Glasgow Coma Scale has been developed; however, results from this scale can be questionable (see Figure 2). It is vital that an accurate and thorough history be obtained, particularly the period of 3–7 days prior to the time the infant presents to medical professionals.

Nurses should ask questions that assess the social history of the family, in addition to the family and medical history of the infant. Source: National Center for Shaken Baby Syndrome (NCSBS). Nurses can also offer parents the following tips for dealing with a crying baby:. Check the baby for signs of illness, teething, or a dirty diaper and resolve those problems if possible. Sing to or talk to the baby.
Glasgow Coma Scale
Take the baby for a walk or a ride in the car, if the caregiver is calm enough to drive. Offer the baby a pacifier. Gently rock the baby or rub his or her back. Parents and caregivers must understand that they may not be able to console the baby and that an inconsolable baby does not make them bad parents or incompetent caregivers.
Mohamed Labib Ahmed El Moghier
In cases where parents cannot stop a baby from crying, they should place the baby on his or her back in a safe crib and step away. They can call a friend, a relative, or a parent support group to seek reassurance. After 10 or 15 minutes, they should check on the baby. If their frustration has subsided, they can once again pick up the baby and attempt to comfort the child. If the frustration and stress are still present, the caregivers should soothe the infant for a moment, without picking the infant up, and then walk away for another 10 or 15 minutes.
Prevention Is Key Abusive head trauma and SBS often result in death and disability in otherwise healthy children and devastate families. The abuse also taxes the healthcare system and resources. Serious brain injury in children has been estimated to consume billions of dollars in healthcare each year. Costs of SBS are significant. Some experts estimate initial hospitalization costs at more than $150,000 and costs of lifetime care at more than $15 million.
Fortunately, SBS is a completely preventable injury, and nurses play an important part in decreasing the incidence of this type of abuse. Many states have enacted their own prevention programs to reduce the incidence of SBS. For example, Kentucky initiated the HANDS program, in which a visitor provides support and information to parents beginning during pregnancy and lasting until their infant is 3 months old.
The goals of the HANDS program are healthy pregnancies and births; healthy child growth and development; healthy, safe homes; and self-sufficient families. Other similar home visitation programs have shown positive results in high-risk families. National-level agencies and organizations also can provide assistance to parents and caregivers to help prevent SBS. As healthcare professionals, nurses can share the following resources with parents so they can keep their children safe: National Center on Shaken Baby Syndrome provides information and training related to SBS. Their initiative titled The Period of Purple Crying Program is child-abuse prevention program that includes a booklet and DVD for parents and caregivers. Another initiative, the Dads 101 Program, is an education program targeting new and expectant fathers.
Presented by a male instructor, the program offers instruction in basic caregiving skills and provides a venue for fathers to express their concerns about parenthood. You can find more about these programs at www.dontshake.org. Centers for Disease Control and Prevention (CDC) published a guide for healthcare professionals titled Preventing Shaken Baby Syndrome: A Guide for Health Departments and Community-Based Organizations that outlines basic facts about SBS and suggestions for public prevention efforts that communities can initiate. You can find this publication. The Shaken Baby Alliance was established in the late 1990s by three mothers whose children suffered from SBS.
The mission of the alliance is to provide support for victim families and professionals, prevent child abuse, and seek justice for the victim of child abuse. Educational materials can be found on their Web site at www.shakenbaby.org. Circle of Parents is an online network of parent-led support groups that provides a place for parents to share ideas and address challenges of parenting. The network is located at All Babies Cry, a DVD and interactive booklet developed by Vida Communications, provides parents with information about the causes of infant crying, strategies for coping with crying, and helpful tips for parent self-care, including nutritional and sleep advice. This resource is available. A Controversial Diagnosis In recent years, the diagnosis of SBS has come under scrutiny, bringing forth debates among healthcare experts and lawyers.
Although many people think that prosecuting perpetrators of suspected abuse can only benefit society and the victims, others believe that SBS is too-frequently diagnosed, resulting in innocent people being convicted of abuse and sent to prison. Norman Guthkelch, the neurosurgeon who first described the injuries indicative of SBS, is one expert who has recently expressed his concern over the frequent diagnosis of SBS. Guthkelch reviewed a case in Arizona, in which a father was convicted of SBS in the death of his son. The infant, who was born with the umbilical cord around his neck, had a history of uncontrolled seizures. Guthkelch's concern was that the child's medical history was ignored in favor of an SBS diagnosis. The doctor who determined the cause of death in this case has also asked the State of Arizona to review the case, saying, 'If I were to testify today, I would state that I believe the child's death was likely the result of a natural disease process, not SBS.'
Researchers continuously contribute to existing medical knowledge, and nurses and other healthcare professionals need to be careful to not rush to judgment in cases of suspected SBS. Protecting children is the most important action of society in cases of suspected abuse; however, healthcare professionals should not adopt an at-all-costs attitude, concluding that every child that presents with certain symptoms is a victim of abuse. The role of the nurse is to advocate for his or her patient–the child–by accurately assessing the patient and administering care in a professional and objective manner. In cases of SBS, discriminating abuse from other conditions can be difficult, and the nurse should consult other members of the healthcare team for assistance in determining the appropriate needs of the child and the family. Reporting Abuse Healthcare professionals are classified as mandated reporters and have a duty to report suspected or confirmed child abuse, including SBS. Nurses and other healthcare professionals need to take care to not place blame for the abuse but to describe objective medical observations and treatments when reporting potential abuse to state authorities. Nurses should not make evaluative statements or diagnoses but should leave the matter of conviction to the criminal justice system.
Nurses should follow state law and facility policy when reporting suspected abuse. State mandates for reporting can be found at the U.S. Department of Health and Human Resources. Protecting the Innocent Connie, the clinic nurse whose quick action helped baby Joshua receive emergency care, called the state child abuse agency and reported her findings after Joshua was transported to the hospital.
Although at the time abuse was not confirmed, Connie fulfilled her duty as a mandated reporter. One morning, several days later, the hospital staff sent Joshua's hospital records to Connie's office. She reviewed the chart, noting the hospital pediatrician's diagnosis of SBS, with subdural hemorrhage, retinal hemorrhage, cerebral edema, and a two fractured ribs evident in diagnostic tests. State investigators were on the case, and criminal charges were pending. Joshua's prognosis would not be clear for some time, but Connie knew he would likely need long-term medical care and therapy. As disheartened as she was to hear about Joshua, Connie realized her value as a nurse, caring for and advocating for her patients. With this in mind, she reviewed the clinic's appointment list and started her work for the day.
SBS is more than a story for the Metro section editor or crime reporter–it's a health story about a tragedy that can be prevented through greater community awareness and education efforts of nurses and other healthcare professionals. Prevention is a community effort that includes recognizing and communicating the risk factors and common characteristics of perpetrators and victims and also sharing ways to lessen the load on parents and caregivers who are under great amounts of stress.
We need to connect the dots between a parent or caregiver's loss of control and other factors in his or her life or community that increase the risk or build protection, including history of abuse in the family or lack of support system or isolation issues. Through prevention, we can help all people live to their full potential.
References and Suggested Readings Caffey J. On the theory and practice of shaking infants. Amer J Dis Child.1972;124:161–9. A journalist's guide to shaken baby syndrome: A preventable tragedy; 2012. Centers for Disease Control and Prevention Web site. Avail at: National Institute of Neurological Disorders and Stroke. NINDS shaken baby syndrome information page.
Bethesda, MD: NINDS; 2012. Avail at: Paiva, WS, Soares, MS, Amorim, RL, de Andrade, AF, Matushita, H, Teixeira, MJ. Traumatic brain injury and shaken baby syndrome. Acta Med Port.2011;24:805–8. Preventing shaken baby syndrome: A guide for health departments and community-based organizations; 2012. Centers for Disease Control and Prevention Web site.
Avail at: Salamon, M. In shaken baby syndrome, women as likely to be perpetrators as men. Avail at: Shapiro, J. Rethinking shaken baby syndrome. New York: NPR; 2011. Avail at: State guides and manuals; 2011. Department of Health and Human Services Web site.
Avail at: www.childwelfare.gov Szalavitz, M. The shaky science of shaken baby syndrome.
January 17, 2012. Avail at: Verive, MJ. Pediatric head trauma. Medscape reference. Avail at: Kentucky Legal Requirement The 2010 Kentucky Legislature amended the 314.073 Nursing Continuing Competency requirements to include a requirement for all nurses to obtain education related to pediatric abusive head trauma, including shaken baby syndrome.
All present and future licensed nurses are required to complete one training course of at least 1.5 hours that includes the recognition and prevention of pediatric abusive head trauma, as defined by Kentucky law. The hours required under this section shall be included in the current number of required continuing education hours. Nurses licensed before July 15, 2010, shall demonstrate completion of this course by December 31, 2013. Nurses licensed on or after July 15, 2010 must receive the education 3 years of their initial licensure dates. Per Kentucky law, nurses, paramedics and emergency medical technicians, physicians, teachers and other school personnel, child care personnel, and law enforcement officers, among other personnel, who knows or has reasonable cause to believe, that a child is dependent, neglected, or abused is required to report the suspicions to the proper law enforcement and government officials. Abuse is defined as interfering with child's right to adequate food, shelter, clothing, education, medical care and freedom from physical, sexual, or emotional injury or exploitation or abandonment.
The National Center for Continuing Education, Inc., is an approved Kentucky Board for Nursing continuing education provider. Transformers playstation game. Successful completion of this course will fulfill the requirement of the Commonwealth of Kentucky.
METHODS A retrospective cohort analysis of patients suffering from severe TBI registered in the Trauma Registry of the German Society for Trauma Surgery between 2002 and 2013 was undertaken. Severe TBI was defined as an Abbreviated Injury Scale of the head (AIS head) score of ≥ 3 and an AIS score for any other part of the body that does not exceed the AIS head score. Only patients with complete data (GCS score, age, and pupil parameters) were included. To assess the impact of GCS score and pupil parameters, the authors also used the recently introduced Eppendorf-Cologne Scale and divided the study population into 2 groups: children (0–15 years old) and adults (16–55 years old). Each patient's outcome was measured at discharge from the trauma center by using the Glasgow Outcome Scale.
RESULTS A total of 9959 patients fulfilled the study inclusion criteria; 888 (8.9%) patients were ≤ 15 years old (median 10 years). The overall mortality rate and the mortality rate for patients with a GCS of 3 and bilaterally fixed and dilated pupils (19.9% and 16.3%, respectively) were higher for the adults than for the pediatric patients (85% vs 80.9%, respectively), although cardiopulmonary resuscitation rates were significantly higher in the pediatric patients (5.6% vs 8.8%, respectively). In the multivariate logistic regression analysis, no motor response (OR 3.490, 95% CI 2.240–5.435) and fixed pupils (OR 4.197, 95% CI 3.271–5.386) and bilateral dilated pupils (OR 2.848, 95% CI 2.282–3.556) were associated with a higher mortality rate. Patients ≤ 15 years old had a statistically lower mortality rate (OR 0.536, 95% CI 0.421–0.814; p = 0.001).
The rate of good functional outcomes (Glasgow Outcome Scale Score 4 or 5) was higher in pediatric patients than in the adults (72.2% vs 63.1%, respectively).